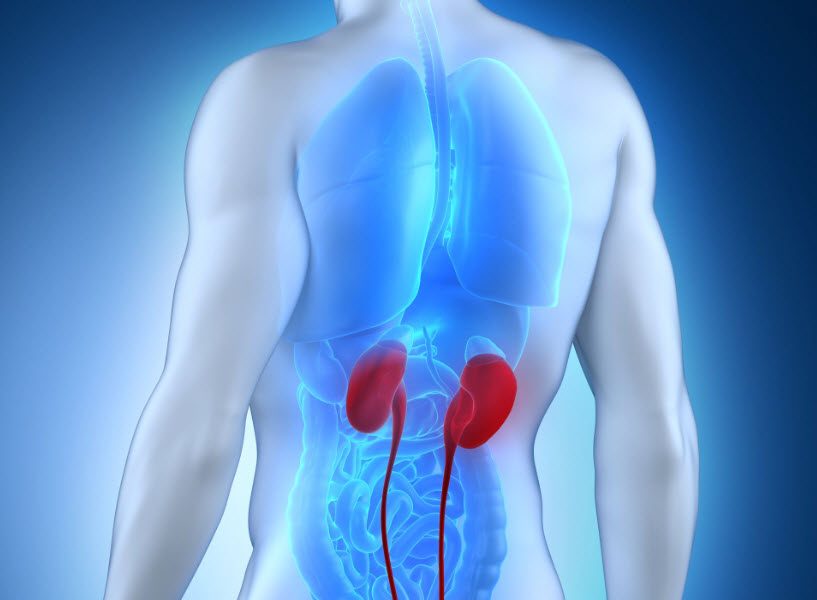
Advancements in the diagnosis and treatment of glomerulonephritis, a group of kidney disorders characterized by inflammation in the glomeruli, have significantly improved our understanding and management of this condition. These developments have allowed healthcare professionals to provide more precise and effective care to patients with glomerulonephritis, ultimately enhancing their quality of life. One notable advancement in glomerulonephritis diagnosis is the utilization of advanced imaging techniques such as ultrasound, computed tomography CT scans, and magnetic resonance imaging MRI. These imaging methods enable healthcare providers to visualize the kidneys and identify structural abnormalities, which can be essential in diagnosing the underlying causes of glomerulonephritis, whether it is primary idiopathic or secondary to another condition, such as systemic lupus erythematosus or diabetes. In addition to imaging, the use of renal biopsy has become more refined, allowing for more accurate and targeted tissue sampling assessing the extent and nature of glomerular damage.
This diagnostic precision facilitates the development of personalized treatment plans. In terms of treatment, several groundbreaking approaches have emerged to better manage glomerulonephritis and its complications. Immunosuppressive therapies, including corticosteroids and immunosuppressive drugs like cyclophosphamide, have proven effective in reducing inflammation and slowing disease progression in some forms of glomerulonephritis. The emergence of novel biologic agents, such as rituximab, has provided additional options for targeted immunomodulation. These therapies aim to suppress the immune system’s overactive response, thereby mitigating inflammation in the glomeruli. Furthermore, advancements in precision medicine have enabled the identification of specific biomarkers associated with different types of glomerulonephritis. This allows for a more individualized approach to treatment, as it helps healthcare providers choose the most appropriate therapy for each patient based on their specific disease subtype and underlying causes. For example, in cases of primary membranous nephropathy, the discovery of autoantibodies against the M-type phospholipase A2 receptor PLA2R and thrombospondin type-1 domain-containing 7A THSD7A has led to targeted therapies directed at these antigens view the site https://massageolie.net/a-comprehensive-guide-to-glomerulonephritis-causes-symptoms-diagnosis-treatment-and-supportive-care. This tailored approach minimizes potential side effects and enhances treatment efficacy.
Additionally, the development of new drugs that target specific inflammatory pathways has shown promise in the management of glomerulonephritis. Janus kinase JAK inhibitors, for instance, are being explored as potential treatments for certain autoimmune forms of glomerulonephritis, such as lupus nephritis. These medications offer a more targeted way to control inflammation, potentially reducing the reliance on broad-spectrum immunosuppressive agents. In summary, advancements in glomerulonephritis diagnosis and treatment have ushered in an era of more personalized and effective care. From improved imaging techniques and precise diagnostic tools to targeted immunosuppressive therapies and emerging biologic agents, the landscape of managing glomerulonephritis has evolved significantly. These innovations not only enhance the accuracy of diagnosis but also enable healthcare providers to tailor treatment strategies to individual patients, optimizing their outcomes and improving their overall quality of life.
Categories: Health